To Ketone or Not to Ketone: Mineral Salts

Ketone Mineral Salts – Key Takeaways:
- Ketone supplements such as ketone mineral salts are exploding in the marketplace. As we begin to see more research about the effects of ketone supplements on a variety of performance, cognitive, and therapeutic applications, it’s important to know the context that the ketone mineral salts are bound to play.
- Don’t fear moderate sodium loads, especially when insulin is low (i.e., low carb or ketogenic dieting).
- Be cautious of ketone mineral salts loading up on calcium for fear of “public perception” of sodium content.
- Magnesium is important for a variety of functions.
- Keep in mind your intake of these minerals via your diet and allow that to help guide your decision on ketone supplements.
- Ketone mineral salts have the potential to provide a dual role, which includes benefits from the ketones themselves and from the minerals they are bound to.
Let me preface this article by stating that I am not affiliated with any ketone or ketone mineral salts company and haven’t tested them in any way. Rather, due to the recent explosion of ketone supplements on the market, I wanted to cover the importance of considering the mineral salt content of these supplements.
 Exogenous ketones are becoming more popular as advancements in scientific research continue to show how they work to improve both health and performance. At first, the only options for delivering exogenous ketones were unpalatable ketone esters; however, exogenous ketones can now be taken in the form of ketone mineral salts that are more palatable and easily blended in water.
Exogenous ketones are becoming more popular as advancements in scientific research continue to show how they work to improve both health and performance. At first, the only options for delivering exogenous ketones were unpalatable ketone esters; however, exogenous ketones can now be taken in the form of ketone mineral salts that are more palatable and easily blended in water.
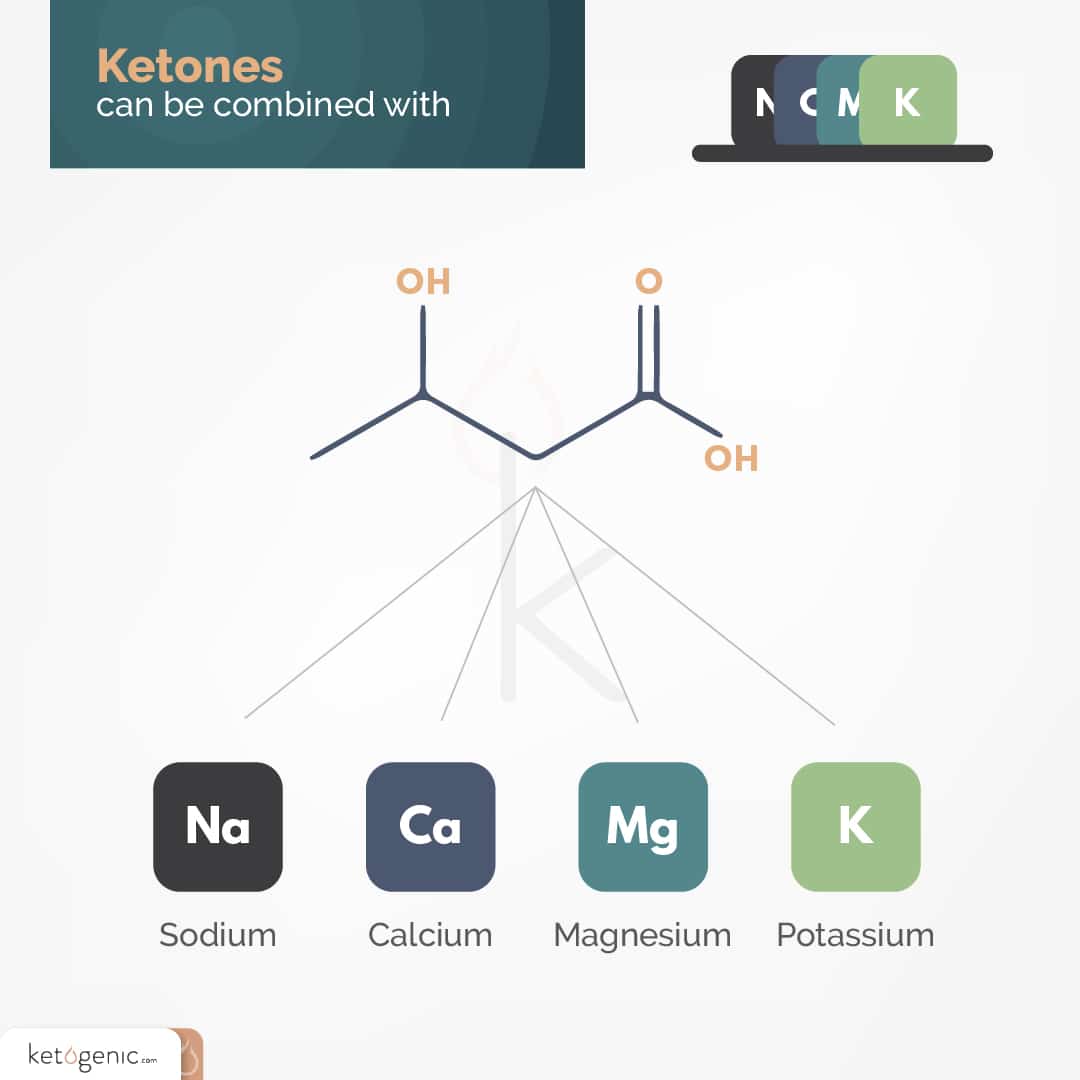
Making ketone mineral salts involves combining beta-hydroxybutyrate (BHB) with mineral salts such as sodium, calcium, magnesium, or potassium, which are also key electrolytes. Before considering whether ketone supplements are a good option, most people immediately look at the salt load, and rightfully so. It is important to take into account the nutritional and health impact of not only the BHB but the minerals that are used to make the product.
The Potential of Ketone Mineral Salts
Although most of the research has been done utilizing ketone esters, ketone mineral salts supplementation has the potential to provide additional benefits through the extra electrolytes/nutrients that are required to make the ketones. While ketone esters are expensive due to the manufacturing process involved in making them, ketone salts might be a more convenient option for both inducing a state of ketosis and elevating blood ketone levels for various reasons we will discuss in another article.
Let’s take a look at some of the facts and misconceptions about three of the minerals used to make ketone mineral salts: sodium, calcium, and magnesium. Potassium is very hygroscopic, meaning that it absorbs water very easily. Therefore, it is only feasible that it can be utilized in liquid formulations. Thus, one should be cautious if companies say they have potassium BHB salt powder in their product. I’d be very surprised if that’s actually the case.
Sodium
We’ve all been taught that high sodium intake is bad for us, similar to how we’ve been told for decades that fat is the driver of coronary heart disease, and consuming large amounts will kill us. Sodium has been thought to increase blood pressure, and therefore increase the risk of heart disease, kidney disease, stroke, osteoporosis, and stomach cancer. Thus, many of us tend to avoid consuming foods or supplements with labels that have high amounts of sodium.
There are two problems with this approach:
- We tend to focus on the wrong foods and forget about the ones that have the highest amount of sodium content.
- For many of us, high sodium intake is actually not a bad thing. In fact, there is evidence that the current USDA recommendations for sodium intake are too low.
Looking in the Wrong Places
People often put down food choices because the sodium content is too high. Canned soup with 890 mg of sodium? I’ll pass. Ketone mineral salts with 900 mg of sodium? No way!
Recently, a friend of mine’s dad had high blood pressure. His doctor told him to stop consuming eggs and to avoid adding extra salt to his foods. That’s it. His recommendation was to rid a good, high-quality protein source, yet French fries, chicken nuggets, and even chicken noodle soup were all presumably okay. I’ll never understand some of these recommendations; nonetheless, they happen day in and day out, all over the world.
The culprit is often restaurant meals or other meals where the nutrition facts are not available with the food itself. Such “ignorance is bliss” situations allow us to avoid dealing with daunting numbers. Many people don’t hesitate to stop and enjoy a meal at a restaurant, but they freak out when they actually see the numbers on a label. By now, we all know that opting for fatty meat with a side of veggies cooked in butter isn’t that bad after all. It turns out that what you thought to be the safe, “healthy,” doctor-approved choice might not always be what you think it is.
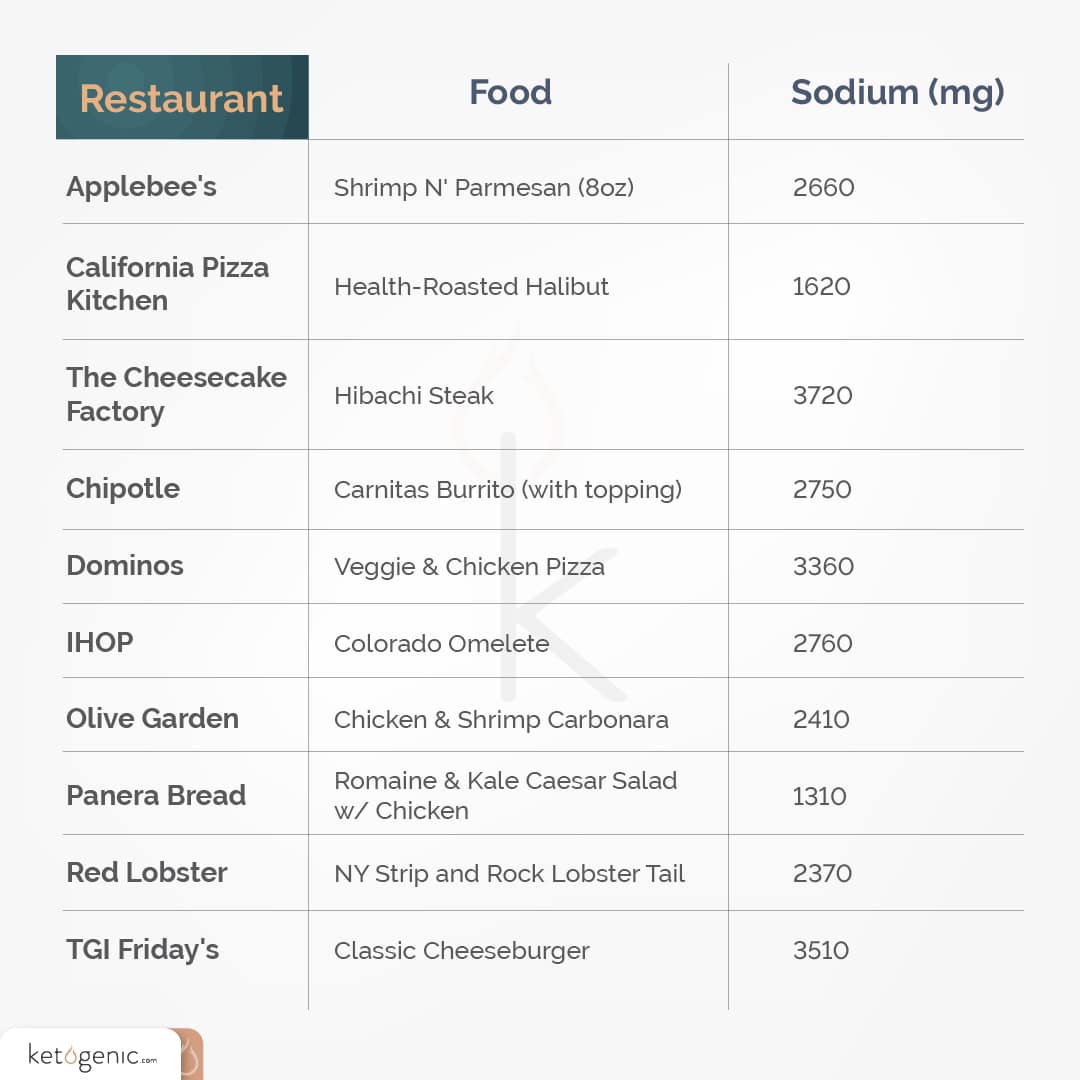
Here are a few examples of the sodium content in high-protein menu options at some popular American restaurants:
These aren’t even the highest options on each menu! Some items have up to 4000 mg sodium or more, and that’s just for one meal. If you truly want to stay away from high-sodium menu options, you might want to think twice about your heart-healthy, whole wheat breakfast pancakes with maple syrup, or whole wheat wrap and fries for lunch.
So why are restaurant foods so high in sodium? For most of the above restaurants, the food is made ahead of time, and high-sodium foods and condiments are piled on top of each other. But maybe we shouldn’t be so alarmed at some of these higher numbers, especially when eating a lower carbohydrate or even ketogenic diet.
Looking for the Wrong Culprit
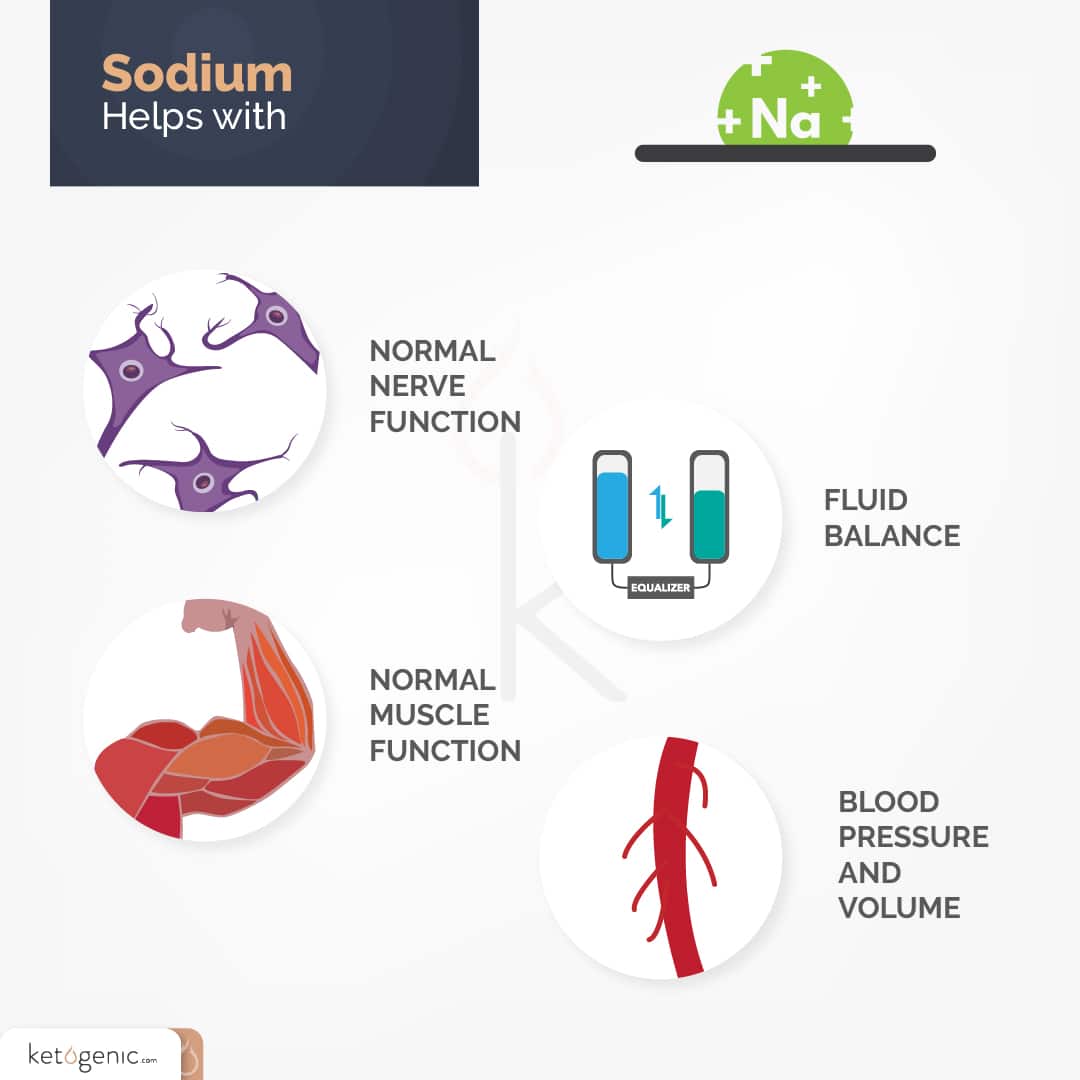
Many of us have heard the saying, “Don’t blame the butter for what the bread did.” Similarly, don’t blame the sodium for what the fries did. Sodium has been shown to help maintain fluid balance, normal muscle and nerve function, and blood pressure and volume. [1] The movement of sodium ions and other electrolytes across cell membranes helps to facilitate muscle contraction and nerve impulses. Electrolytes also help to maintain fluid balance across intracellular and extracellular spaces and blood volume.
Acutely, high sodium intake will likely make you thirsty, and low sodium intake will likely make you tired. At a minimum, we need at least 500 mg sodium a day to survive. [2] For many years, we have placed too much attention on excess sodium and perhaps not enough on excess intake of other minerals, or whether or not we are getting enough sodium.
Many of us avoid foods like processed meats and cheeses or salted nuts because of their high sodium content. However, processed carbohydrate sources can have equal or higher amounts of sodium per serving. An ounce of salted pretzels [3] has over four times as much sodium as an ounce of salted peanuts. [4] Just because we can’t taste the sodium doesn’t mean it isn’t in there. Flavors from other ingredients like sugar and spices can make it difficult to identify salt as a dominant flavor.
Are You Getting Enough?
The USDA guidelines recommend less than 2400 mg of sodium per day for healthy adults, and 1500 mg or less for individuals over the age of 50 or at risk for hypertension. [2] For reference, 2300 mg of sodium is the equivalent of about one teaspoon of salt. Even though these recommendations are promoted by the American Heart Associated and other health-related organizations, recent research has claimed that there is simply not enough evidence to support these guidelines. [5] Worldwide 24-hour urinary sodium excretion data suggest that the normal range is actually 2500-5000 mg per day, which is what most of us consume daily. [6] Additionally, people with high activity levels or chronically low blood pressure may require more sodium than the average person.
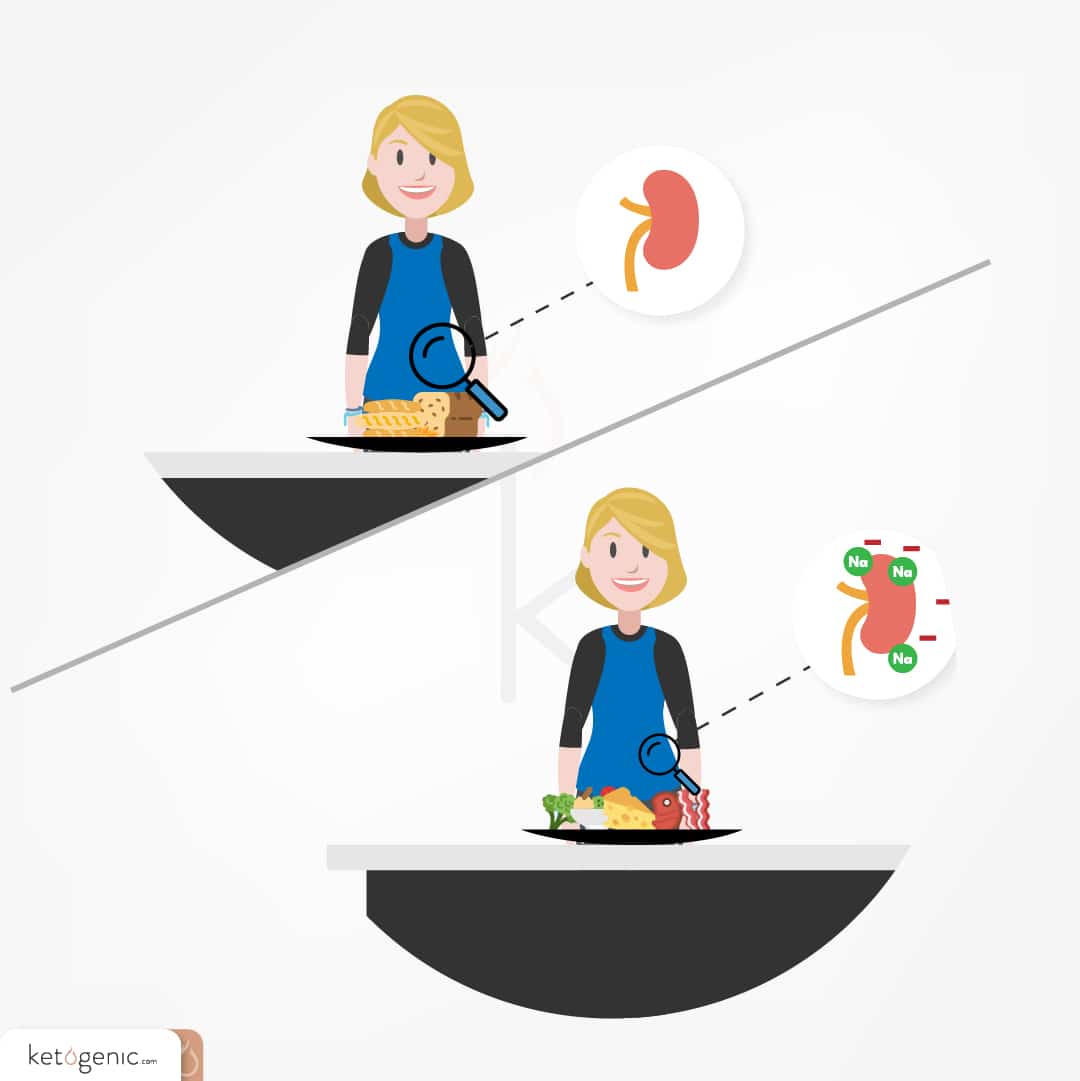
There is also evidence that individuals who adhere to a low-carbohydrate or ketogenic diet may require higher sodium intakes. Due to their low carbohydrate contents, these diets reduce insulin levels. Since one of insulin’s roles is to decrease the excretion of sodium in the urine, [7] low-carbohydrate and ketogenic dieters excrete more sodium than normal, and are encouraged to salt their meals to increase their sodium intake.
Too low of sodium intake can be just as dangerous as getting too much. As with all essential nutrients, the graph for risk associated with sodium and health problems is actually u-shaped, such that both low and high quantities of sodium are associated with risk of cardiovascular disease and all-cause mortality. [8] Evidence also suggests that restricting sodium to the recommendations may rapidly increase plasma levels of renin, angiotensin II, and aldosterone, which can lead to complications in itself. [9]

Don’t Fear Sodium
The current USDA recommendations reflect “unachievable goals” that do not match what research suggests our normal physiological ranges might be. [10] There is not enough evidence to show that sodium restriction is associated with less mortality or cardiovascular morbidity in healthy individuals or individuals with high blood pressure, and there is evidence that sodium restriction might actually be harmful to individuals with heart failure. [11] For serious athletes, and individuals who are active daily, the current recommendations might not only be unwise but unsafe. If you are eating a carbohydrate-restricted diet, this applies to you even more. Don’t stress about the high amounts of sodium in a lot of these ketone mineral salt supplements, being that they allow for a fast delivery of ketones to the body, which has unique benefits that will be discussed in a separate article. Instead, change out the frozen dinner and experiment with an effective dose of exogenous ketones.
Calcium
We are told by our parents, doctors, and the media that milk builds strong bones and that we should take calcium supplements to help protect against osteoporosis. Indeed, calcium deficiency can lead to a plethora of health problems. [12] However, those of us who take calcium supplements or consume calcium-fortified foods and beverages may, in fact, be consuming above the Recommended Dietary Allowance (RDA) of calcium.
In a society where everything is supersized, the question has transitioned from, “Are we consuming enough?” to “Are we consuming too much?”
Too Much Calcium?
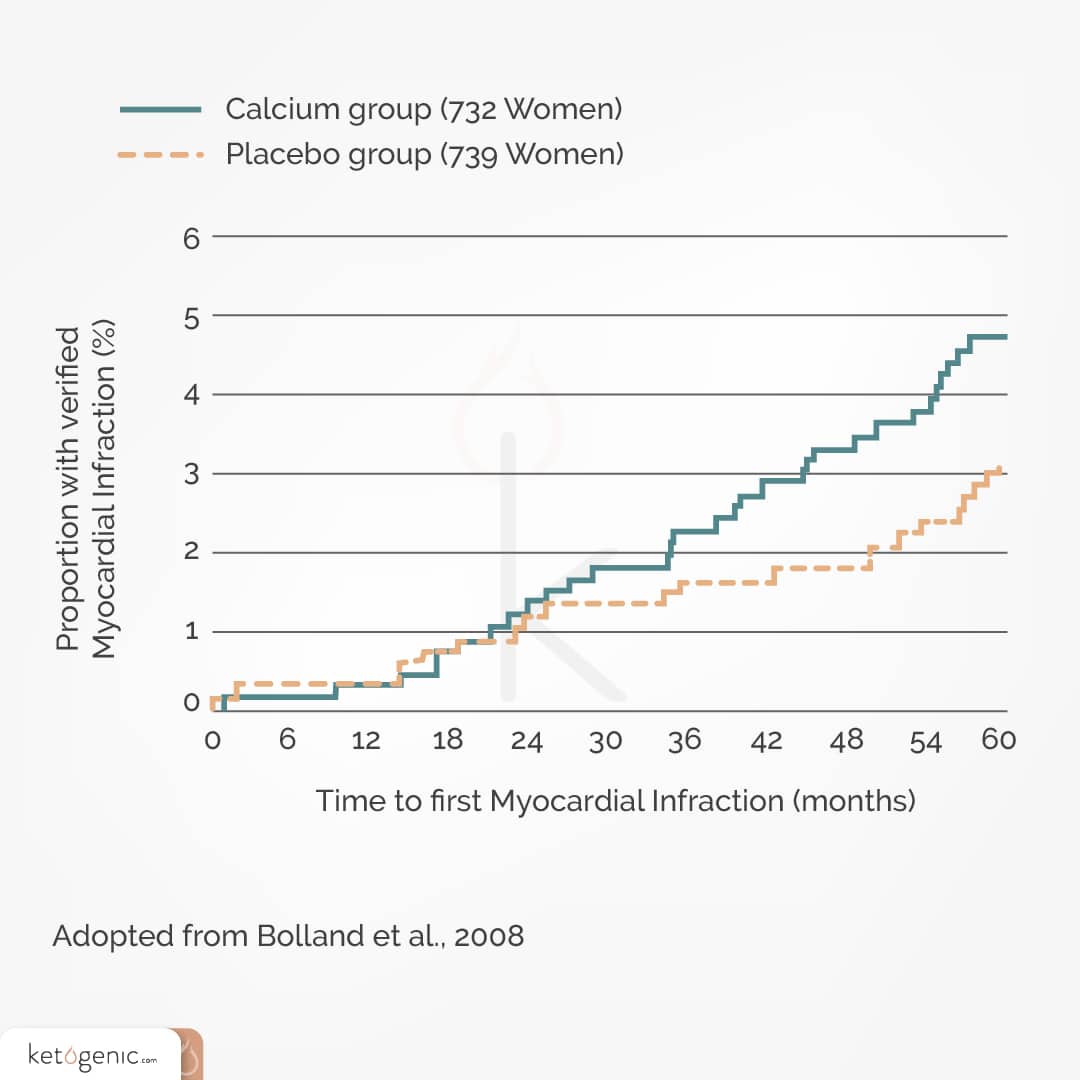
Look around your grocery store, and you’ll soon start to see “Fortified with Calcium” on a variety of different labels, along with calcium supplements everywhere you look. Calcium is essential for cardiovascular health, but several studies have found too much calcium to be associated with cardiovascular events and even death. One study found that consumption of 1000+ mg of supplemental calcium per day was associated with an increased risk of death from cardiovascular disease in men but not women. [13] Dietary calcium intake (i.e., calcium from incorporated foods such as milk, etc.), on the other hand, was not associated with death from cardiovascular disease in men or women. Additionally, a different study found 1000 mg of supplemental calcium to be associated with an increase in rates of cardiovascular events in women. [14]
Increased calcium levels in the bloodstream may contribute to the hardening of arteries (atherosclerosis), which in turn can lead to a heart attack. Calcium from supplements enters the bloodstream in one bolus, whereas we usually tend to get calcium from foods in small doses from the breakdown process. This might explain why calcium from food doesn’t create the same risk that is introduced by calcium supplements. At first glance, it seems to be the case that high calcium intake –at least from supplements–may not be ideal.
Food vs. Supplements
As stated above, there appears to be a difference between supplemental and dietary calcium intake, which can be important to keep in mind. One study found aggregate calcium intakes above 1400 mg per day (from dietary and supplemental intake combined) to be associated with higher death rates, cardiovascular disease, and ischemic heart disease in women. [15] A 2014 meta-analysis found an association between dietary calcium intake and cardiovascular mortality. [16] The meta-analysis actually found a u-shaped relationship, where dietary calcium intakes that were both lower and greater than 800 mg/day were gradually associated with increased risk of cardiovascular mortality.
At the same time, research suggests that getting as much of your calcium from your diet, rather than supplements is a good idea. For instance, there is some evidence that the calcium intake from food is better for bone mineral density than the same calcium intake from supplements. [17] Foods that are high in calcium include dairy, leafy green vegetables, fish with edible bones, tofu made with calcium sulfate, and calcium-fortified foods and beverages.
Lack of Reliability
Although several studies have linked calcium supplementation with an increased risk of heart attack and heart disease, [18] other studies have not found the same association. For example, a study on calcium supplementation (1000 mg/day) in postmenopausal women indicated a reduced risk of hip fracture, but no increase in cardiovascular disease or mortality in the supplement group, compared to the placebo group. [19] Another study found no effect from calcium supplementation (600 or 1200 mg/day) on abdominal aortic calcification. [20]
Even though there is mixed evidence regarding the association between calcium supplementation and cardiovascular events, there may be other reasons to avoid high calcium supplementation. In one of his studies, Dr. Bolland claimed that calcium supplements do not prevent hip fractures. Rather, they may lead to kidney stones, acute gastrointestinal events, and increased risk of myocardial infarction and stroke. Thus, the risks involved with high-calcium supplementation potentially outweigh the benefits. [21]
The research at this point is inconclusive. Nevertheless, the findings so far are cause for concern and a reminder that more calcium isn’t necessarily better.
The Safe Zone
Currently, we lack enough evidence to change the recommendations for calcium intake. The Tolerable Upper Intake Level (UL) for adults 19-50 years old is 2500 mg. This is well over the RDA of 1000 mg for the same age group. Calcium supplements commonly contain 600-1200 mg. When assessing your own calcium intake, keep in mind that calcium from food sources and calcium from supplements may have different outcomes.
Ketone Mineral Salts Supplements and Calcium
It is a good idea to weigh the pros and cons before deciding to add a calcium supplement to your diet. This includes exogenous ketone supplements and ketone mineral salts. If you have any risk factors for osteoporosis, have low bone density, or have issues that prevent you from consuming a nutrient-rich diet, then the benefits of calcium supplements will likely outweigh the risks. But don’t forget that there are other avenues to improving your bone density, like strength training, and, more importantly, a well-balanced diet.
This research is a good reminder to discuss with your doctor before taking any supplements. Given the widespread use of calcium supplements, more research is required before any final conclusions can be drawn. Several ketone companies have tried to avoid the large sodium loads but instead relied on a bump in the calcium content from the BHB ketone mineral salts, seemingly without consideration for the aforementioned results. Calcium BHB will likely absorb slower compared to sodium BHB due to digestion and absorption kinetics. For those looking to optimize brain uptake of ketones, this probably isn’t the best strategy (as uptake is directly proportional to the levels in the blood). Be cautious of supplements running from the sodium and chasing the calcium BHB instead, and make sure you factor that into your overall daily needs.

Magnesium
Magnesium has been called an “orphan nutrient” compared to calcium, which has been a focus in research and media for years. Yet, nearly half of us might not be getting enough magnesium. [22]
Why We Need Magnesium
The many roles of magnesium include helping us maintain normal nerve and muscle function, as well as heart rate, supporting a healthy immune system, regulating blood glucose levels, and making energy production and protein synthesis possible. [23] Magnesium is also involved in both aerobic and anaerobic energy production. ATP synthesis (the body’s energy source) depends on enzymes that are activated by magnesium.
Low magnesium levels and high calcium-to-magnesium ratios may be associated with inflammation-related disorders like type 2 diabetes, metabolic syndrome, and osteoporosis. [22] Increasing magnesium intake is associated with a reduced risk of diabetes, stroke, heart failure, and even death. [24]
How Much Do We Need?
The current recommendation for magnesium is 310-320 mg for adult women and 400-420 mg for adult men. Magnesium deficiencies are common; 2005-2006 data indicates that the majority of Americans’ dietary magnesium intake was less than the Estimated Average Requirement (EAR) for the respective age groups. [25] The EAR for a nutrient is about 20% LESS than the RDA. Current data on magnesium intake and deficiency in the US is not readily available, as magnesium testing is not part of routine electrolyte testing in hospitals and clinics. [26]
Athletes and Magnesium
While we need magnesium to maintain normal health, athletes can also benefit from magnesium by improving performance and recovery. Magnesium supplements have been shown to improve strength [27] [28] and muscle metabolism. [27]
Additionally, athletes are at risk for magnesium deficiency due to increased sweating and urination, and in some cases decreased intake. [29] Magnesium deficiency is associated with increased insulin resistance [30] and decreased athletic performance. [31]
Still More to Learn
If you truly want to optimize health and performance, magnesium should not be neglected. There is still more research to be done on its potential. Good sources of magnesium include whole grains, nuts, seeds, legumes, green leafy vegetables, and supplements. However, be careful about taking too much magnesium at one time, or else you might end up running to the bathroom in a hurry.
References
American Heart Association. Sodium and your health. Version current 27 December 2016. Internet: https://sodiumbreakup.heart.org/sodium_and_your_health (accessed 27 December 2016).
American Heart Association. How much sodium should I eat per day? Version current 7 December 2016. Internet: https://sodiumbreakup.heart.org/how_much_sodium_should_i_eat (accessed 7 December 2016).
Self NutritionData.Snacks, pretzels, hard, plain, salted. Version current 27 December 2016. Internet: http://nutritiondata.self.com/facts/snacks/5367/2 (accessed 27 December 2016).
Self NutritionData. Peanuts, all types, oil-roasted, with salt. Version current 27 December 2016. Internet: http://nutritiondata.self.com/facts/legumes-and-legume-products/4357/2 (accessed 27 December 2016).
McGuire S. Institute of Medicine. 2013. Sodium intake in populations: assessment of evidence. Washington, DC: The National Academies Press, 2013. Adv Nutr 2013;5:19-20.
McCarron DA, Kazaks AG, Geerling JC, Stern JS, Graudal NA. Normal range of human dietary sodium intake: a perspective based on 24-hour urinary sodium excretion worldwide. Am J Hypertens 2013;26:1218–23.
Tiwari S, Riazi S, Ecelbarger CA. Insulin’s impact on renal sodium transport and blood pressure in health, obesity, and diabetes. Am J Physiol-Renal 2007;293(4):F974-84.
Alderman MH, Cohen H, Madhavan S. Dietary sodium intake and mortality: the National Health and Nutrition Examination Survey (NHANES I). Lancet 1998;351(9105):781-5.
Graudal NA, Galløe AM, Garred P. Effects of sodium restriction on blood pressure, renin, aldosterone, catecholamines, cholesterols, and triglyceride: A meta-analysis. JAMA 1998;6:1383-1391.
McCarron DA, Geerling JC, Kazaks AG, Stern, JS. Can dietary sodium intake be modified by public policy?. Clin J American Soc Nephrol 2009;4(11):1878-2.
Taylor RS, Ashton KE, Moxham T, Hooper L, Ebrahim S. Reduced dietary salt for the prevention of cardiovascular disease. Cochrane Database Syst Rev 2011; 7(7).
National Institutes of Health. Calcium: dietary supplement fact sheet. Version current 27 December 2016. Internet: https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/#h5 (accessed 27 December 2016).
Xiao Q, Murphy RA, Houston DK, Harris TB, Chow WH, Park Y. Dietary and supplemental calcium intake and cardiovascular disease mortality: the National Institutes of Health-AARP Diet and Health Study. JAMA Intern Med 2013;173(8):639-646.
Bolland MJ, Barber PA, Doughty RN, Mason B, Horne A, Ames R, Gamble GD, Grey A, Reid IR. Vascular events in healthy older women receiving calcium supplementation: randomized controlled trial. BMJ 2008;336:262.
Michaelsson K, Meihus H, Lemming EW, Wolk A, Byberg Long term calcium intake and rates of all-cause and cardiovascular mortality: community based prospective longitudinal cohort study. BMJ 2013;346:f228.
Wang X, Chen H, Ouyang Y, Liu J, Zhao G, Bao Dietary calcium intake and mortality risk from cardiovascular disease and all causes: a meta-analysis of prospective cohort studies. BMC Medicine 2014;12:158.
Napoli N, Thompson J, Civitelli R, Armamento-Villareal Effects of dietary calcium compared with calcium supplements on estrogen metabolism and bone mineral density. Am J ClinNutr 2007;85:1428-1433.
Lutsey PL, Michos, ED. Vitamin D, calcium, and atherosclerotic risk: evidence from serum levels and supplementation studies. CurrAtheroscler Rep 2013;15(1): 293.
Prentice RL, Pettinger MB, Jackson RD, et al. Health risks and benefits from calcium and vitamin D supplementation: Women’s Health Initiative clinical trial and cohort study. Osteoporosis Int 2013;24(2):567-580.
Wang TK, Bolland MJ, Pelt NC, Horne AM, Mason BH, Ames RW, Grey AB, Ruygrok PN, Gamble GD, Reid IR. Relationships between vascular calcification, calcium metabolism, bone density and fractures. J Bone Miner Res 2010;25:2777–85.
Bolland MJ, Grey A, Reid IR. Calcium supplementation and cardiovascular risk: 5 years on. TherAdv Drug Saf 2013;4(5):199-210.
Rosanoff A, Weaver CM, Rude RK. Suboptimal magnesium status in the United States: are the health consequences underestimated? Nutr Rev 2012;70(3):153-64.
National Institutes of Health. Magnesium: fact sheet for health professionals. Version current 27 December 2016. Internet: https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/ (accessed 27 December 2016).
Fang X, Wang K, Han D, He X, Wei J, Zhao L, Imam MU, Ping Z, Li Y, Xu Y, Min J, Wang F. Dietary magnesium intake and the risk of cardiovascular disease, type 2 diabetes, and all-cause mortality: a dose-response meta-analysis of prospective cohort studies. BMC Med 2016;14(1):210.
Moshfegh A, Goldman J, Ahuja J, Rhodes D, LaComb What we eat in America, NHANES 2005-2006: Usual nutrient intakes from food and water compared to 1997 Dietary Reference Intakes for vitamin D, calcium, phosphorus, and magnesium. 2009. U.S. Department of Agriculture, Agricultural Research Service.
Rude RK. Magnesium. In: Coates PM, Betz JM, Blackman MR, Cragg GM, Levine M, Moss J, White JD, eds. Encyclopedia of Dietary Supplements. 2nd ed. New York, NY: Informa Healthcare, 2010:527-37.
Lukaski, HC. Magnesium, zinc, and chromium nutriture and physical activity. Am J ClinNutr 2000;72(2):585s-593s.
Brilla L, Haley T. Effect of magnesium supplementation on strength training in humans. J Amer Coll Nutr 1992;11(3):326-329.
Nica AS, Caramoci A, Vasilescu M, Ionescu AM, Paduraru D, Mazilu Magnesium supplementation in top athletes – effects and recommendations. MedicinaSportiva 2015;11(1):2482-2494.
Nadler JL, Buchanan T, Natarajan R, Antonipillai I, Bergman R, Rude R. Magnesium deficiency produces insulin resistance and increased thromboxane synthesis. Hypertension 1993;21(6 Pt 2):1024-9.
McDonald R, Keen C. Iron, zinc, and magnesium nutrition and athletic performance. Sports Med 1988;5:171-184.







Miriam, Thank you for the questions. I am going to do my best here to provide you with answers:
Q: The manufacture of BHB salts involves ionic bonding of an anion (beta-hydroxybutyrate) with a cation (Na+, K+, Ca+, Mg+).
At least one of the exogenous ketone products you listed does in fact contain potassium ions. People taking potassium-sparing drugs need to know this and that raises concerns about leaving it off your chart.
A: The table lists the BHB and the mineral content from the BHB salts (no added minerals). Therefore, since potassium BHB is not in any of the products, it wasn’t listed. Some products may add more or less of these, but we should have clarified that this mineral load was intended from the BHB itself.
Q: Some people are genuinely sodium sensitive even to small amounts of salt added to otherwise healthy foods. This can hold true even for those following ketogenic diets.
The term you’re looking for is “hygroscopic” (readily attracts water).
A: This is true, however most people on a ketogenic diet need to increase sodium intake due to increased excretion. For those that are genuinely sodium sensitive, any product or some of the food items listed (i.e even some salads at major food chains) may not be warranted.
Q: The study linking calcium intake to CVD and mortality shows correlation but not causation. That “too little or too much is not good for you” is most likely true, especially in a bolus, so why single out calcium?
I wouldn’t want to put too much stock in a study that supplemented calcium but not magnesium (or D3 or K2…).
My advice to those with low bowel tolerance of magnesium: avoid magnesium oxide, the cheap and poorly absorbed form that’s added to many vitamin and mineral supplements. Magnesium glycinate is well absorbed and better tolerated. Of course, it’s ideal if we’re getting enough from foods but this is difficult to achieve.
Although calcium, sodium, and potassium ions can be assessed in blood, magnesium is trickier given that blood levels are a poor proxy for tissue levels. RBC Magnesium is a better (though not perfect) test.
A: The minerals traditionally used in the formation of BHB are straight calcium or magnesium. They aren’t bound (i.e magnesium glycerinate bound to BHB, but rather straight magnesium bound to BHB).
Q:The “Calcium Could Cause…” graphic is scary, but that graphic (minus the kidney stones) could also be used by those who believe “Fat Could Cause…” Why come head-to-head with those who have exploited bad science?
A: This graphic has since been updated. Excess amounts of calcium, if not properly absorbed and regulated may lead to complications. The article points this out since ketone supplement companies are afraid of elevated sodium levels so some tend to increase calcium to a greater degree feeling that it is completely “safe” regardless of the amount. Acadia’s explanation is meant to just raise awareness on how we just need to take these mineral loads in context, whether we believe them to be healthy or not.
KetoForce claims to have more 1.6 grams each of potassium and sodium BHB salt in each dose of their ketone salt product. Your article says you doubt that the potassium salt is a true ingredient listing. What would they have substituted for it that they could still label as potassium BHB?
I recently purchased InstaKetones potassium BHB with no sodium, calcium, or magnesium identified on the ingredients. The nutrition label lists 3500 mg (3.5 grams) of potassium. Finding information about potassium-bound ketones has been challenging. Can anyone point me in the direction of some reliable information?