Improving Your Gut Health: Why Intestinal Cells Love Ketone Bodies
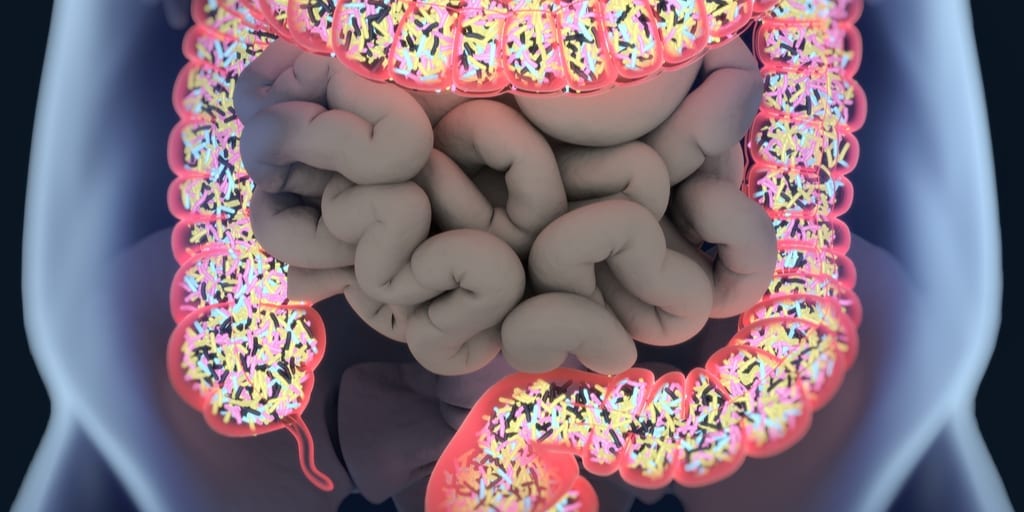
Many factors contribute to a well-functioning, healthy gastrointestinal (GI) system, and a healthy GI system is required for optimal immune function, brain health, and the well-being of every tissue in our body. Building and maintaining a diverse microbiome is one element of having an unimpaired GI system. Another element is growing and maintaining healthy cells that line the GI tract. These cells are called intestinal epithelium cells and may be termed “enterocytes” if they are located in the small intestine, or “colonocytes” if they are located in the colon or large intestine. Interestingly, intestinal cells are shed and renewed every few days.
[block-text]
Why Are Intestinal Cells Important?
These intestinal cells are extremely important, as they play many physiological roles, including [1]:
- Absorbing nutrients from the foods we eat to supply all of our tissues with fuel.
- Facilitating movement of electrolytes and water into our bloodstream.
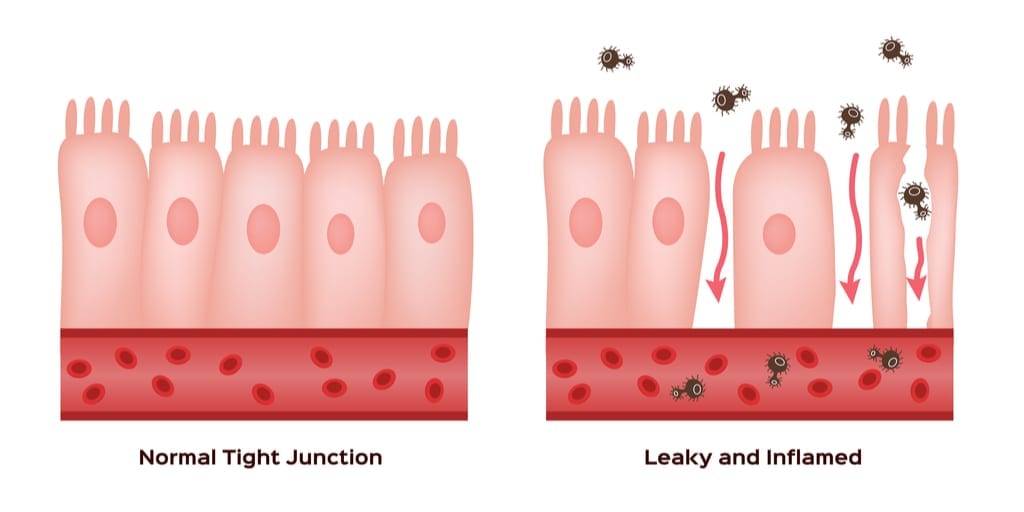
- Providing a barrier to keep harmful substances (i.e., toxins, bacteria) from entering the bloodstream.
- Setting off an immune response if needed to defend against a harmful pathogen.
- Maintaining proper permeability to prevent leaky gut syndrome–a leaky gut occurs when large particles slide between intestinal cells to enter the bloodstream and possibly cause inflammation.
[/block-text]
Intestinal cells absorb nutrients to feed other bodily cells, but what fuels the intestinal cells so that they are able to effectively fulfill the important roles just mentioned? The primary sources of fuel for intestinal cells are glutamine and ketone bodies, especially in the fasted state [2]:
- Absorbing nutrients from the foods we eat .
The Role of Ketones
Regardless of the dietary condition, fatty acids and glucose typically do not make up any major fuel sources for intestinal cells [2].
Although most ketone bodies are primarily produced in the liver, one ketone body can be produced in the colon. In the colon, short-chain fatty acids (SCFAs) are produced when the bacteria in the colon ferment non-digestible carbohydrates (i.e., fiber). SCFAs include acetate, propionate, and butyrate. Butyrate is also a fuel source for colonocytes. However, some of the butyrate in the colon converts to the ketone body acetoacetate. Therefore, a ketone body is also produced indirectly in the colon by the bacteria and then used for fuel by the surrounding colonocytes [3].
The Role Of Glutamine
Diabetes may alter the fuel sources utilized by intestinal cells. Glutamine utilization by intestinal cells decreases proportionally with the length of time one has diabetes. Additionally, with prolonged diabetes, increasing amounts of glutamine are released from skeletal muscle and then taken up by the kidneys and liver, rather than the intestinal cells. This would leave the intestinal cells hungry. However, ketone body utilization increases to partially compensate for the reduced glutamine availability [4].
- Glutamine is a non-essential amino acid (it is not required in the diet, as it can be synthesized naturally by the body) and is the most abundant free amino acid in the body. Thus, glutamine can be obtained by eating protein, but during times of prolonged fasting, it can be provided by bodily protein stores such as skeletal muscle.
- Ketone bodies consist of acetoacetate, beta-hydroxybutyrate, and acetone. They are produced in the liver and metabolized by most tissues, excluding the liver and red blood cells.
Ketone Bodies Fuel Intestinal Cells
To conclude, ketone bodies are a primary fuel source for intestinal cells–both enterocytes and colonocytes, during most physiological conditions. Ensuring that the intestinal cells have an adequate supply of ketone bodies may benefit the health of the intestinal cells. Ketone bodies may be supplied via consuming a ketogenic diet, supplementing with exogenous ketones, and/or eating fiber (non-digestible carbohydrate) to indirectly produce the ketone body acetoacetate in the colon.
References
Henderson, P., van Limbergen, J. E., Schwarze, J., & Wilson, D. C. (2011). Function of the intestinal epithelium and its dysregulation in inflammatory bowel disease.Inflammatory bowel diseases, 17(1), 382-395.
Windmueller, H. G., & Spaeth, A. E. (1978). Identification of ketone bodies and glutamine as the major respiratory fuels in vivo for postabsorptive rat small intestine. Journal of Biological Chemistry, 253(1), 69-76.
Duée, P. H., Darcy-Vrillon, B., Blachier, F., & Morel, M. T. (1995). Fuel selection in intestinal cells. Proceedings of the Nutrition Society, 54(01), 83-94.
Ardawi, M. S. M. (1988). Glutamine and ketone-body metabolism in the gut of streptozotocin-diabetic rats. Biochemical journal, 249(2), 565-572.