You may have heard of insulin resistance and the fact the ketogenic diet may help it, but what does that really mean? Let’s dive into the physiology of this condition, but first, you must understand some basic anatomy and physiology.
An Overview of Pancreas Physiology
The pancreas has both exocrine and endocrine functions. The endocrine portion of the pancreas (islets of Langerhans) secretes insulin, glucagon, and somatostatin, whereas the exocrine portion secretes enzymes that help break down your food.
Endocrine Functions:
-
- Alpha cells of the pancreas secrete glucagon. Glucagon acts in opposition to insulin. Glucagon is released when your blood sugar is low. Glucagon stimulates glycogen breakdown so that it can be released into the blood as glucose and stabilize glucose levels.
- Beta cells of the pancreas secrete insulin. Insulin acts in opposition to glucagon. When blood sugar levels are high, insulin is released to increase cellular uptake of glucose, and thus lower free glucose in the blood.
- Delta cells of the pancreas secrete somatostatin. Somatostatin, also known as growth hormone-inhibiting hormone, blocks the secretion of both insulin and glucagon. Outside of blood glucose regulating effects, somatostatin also has many vital roles including the inhibition of growth hormone by the pituitary gland.
Exocrine Functions:
-
-
- Acinar cells make up the exocrine portion of the pancreas and are responsible for producing enzymes to assist in digesting food.
- Pancreatic proteases, like trypsin and chymotrypsin, break down and digest proteins.
- Pancreatic amylases break down and digest carbohydrates.
- Pancreatic lipases break down and digest fats. [1]
-

What is Insulin?
Insulin is a peptide hormone secreted by the pancreas in response to high blood sugar levels. [2]
How Do Carbs Trigger Insulin Secretion?
When you eat carbohydrate-rich foods, the starches immediately begin digestion in the mouth through both mechanical digestion (chewing) and chemical digestion (from salivary amylases). These carbohydrates travel from the stomach to the duodenum (first part of the small intestine), where they are broken down into monosaccharides (simple sugars). These simple sugars are absorbed in the small intestine and travel through the bloodstream. [3]
Note: Anything that is not absorbed is continued to travel into the colon where it is either broken down by bacteria or continues throughout the colon into the rectum, where it will then be eliminated as stool.
Pancreatic beta-cells detect changes in glucose concentrations and secrete the hormone insulin. Insulin binds to insulin receptors, signaling for glucose uptake within the cell.
Note: Here is a more in-depth overview of insulin secretion. When glucose is transported into beta cells through GLUT2 channels, extracellular fluid (ECF) glucose levels rise. This leads to the depolarization of ATP sensitive K+ channels, which triggers the opening of Ca2/- channels. The influx of calcium increases intracellular fluid (ICF) calcium levels which then triggers margination (insulin storage vesicles move to the cell surface), followed by exocytosis (vesicle fuses to the membrane and releases contents). [4]

Is Insulin Necessary For Glucose To Enter All Cells?
No! Insulin is not required for all cells. Based on the glucose transporter (GLUT) needed to transport glucose into those cells, insulin may or may not be required.
GLUT1
- Cells: blood, blood-brain-barrier, heart
- Insulin-independent (not necessary)
GLUT2
- Liver, pancreas, small intestine
- Insulin-Independent (not necessary)
GLUT3
- Brain, neurons, sperm
- Insulin-Independent (not necessary)
GLUT4
- Skeletal muscle, adipose (fat) tissue, heart
- Insulin-dependent (necessary) [5]
What is Insulin Resistance?
Insulin resistance (IR) describes a reduced response to insulin by cells. Over time, insulin receptors can become desensitized by the signals from insulin. This causes them to respond slowly or not at all. [6]
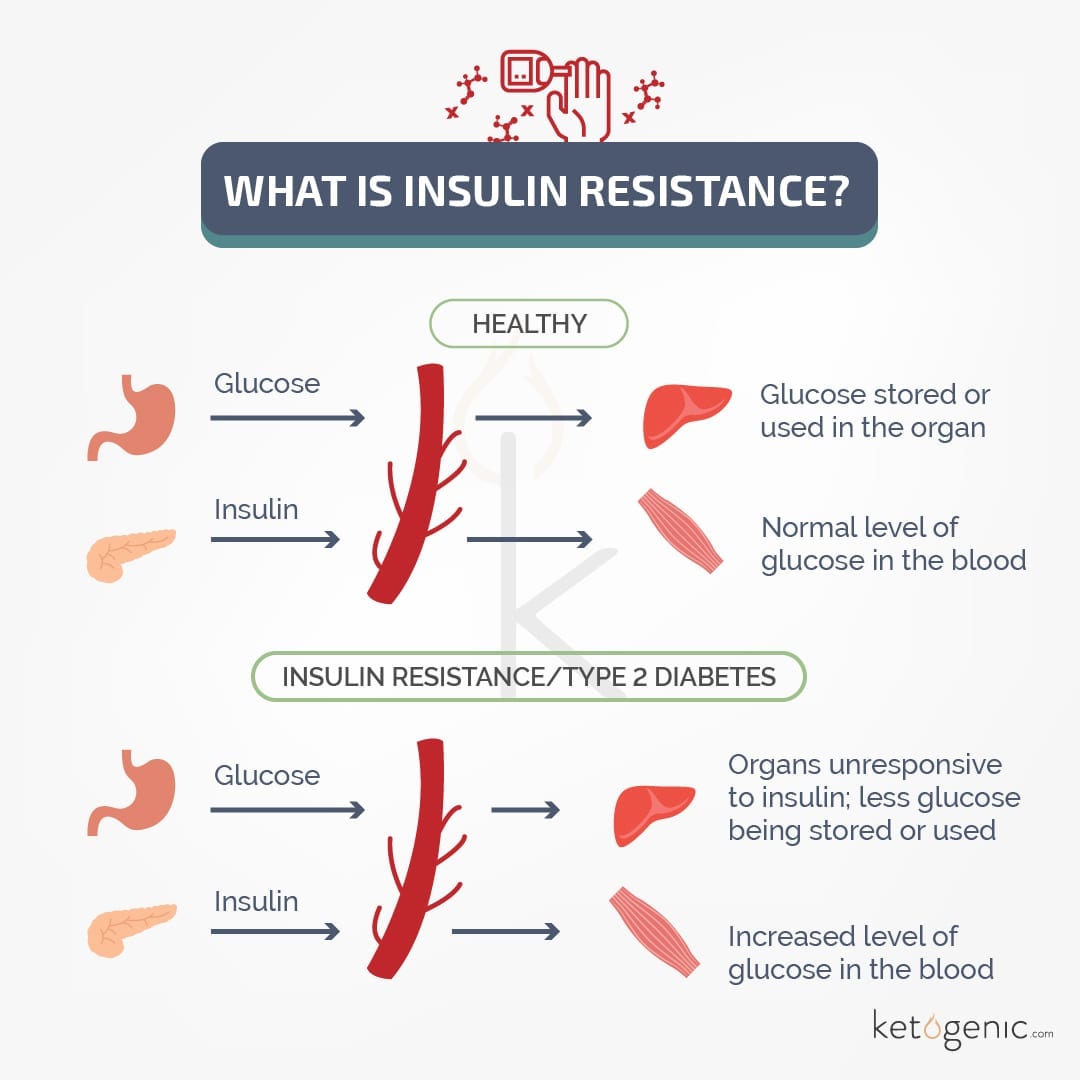
Why is Insulin Resistance Bad/Harmful?
When insulin resistance occurs, glucose can not be taken into cells sufficiently, leaving more glucose floating in the bloodstream, and thus higher blood glucose levels. High blood glucose levels are bad on their own, but to make the matter worse, the pancreas will oversecrete insulin to try and compensate for the high glucose levels. This can wear out beta-cells and cause a decrease in insulin release, very similar to what type 1 diabetes experience.
Type 1 diabetes mellitus is caused by the pancreas secreting too little insulin, whereas type 2 diabetes mellitus is caused by insulin resistance (decreased insulin receptor sensitivity). When insulin levels go unchecked, signaling can become desensitized leading to insulin resistance (type 2 diabetes), but if uncontrolled, pancreatic beta-cells will over-produce insulin, wearing out these cells and leading to the inability to produce sufficient insulin (like in type 1 diabetes).

How Do You Know If You Are Insulin Resistant?
Insulin resistance (IR) is the hallmark of type 2 diabetes. Symptoms of IR include:
- Hyperglycemia (high blood sugar levels)
- Hyperphagia (increased hunger)
- Polydipsia (increased thirst)
- Polyuria (increased urine output)
- Paresthesia (tingling, pricking in hands and feet)
- Lethargy (decreased energy) [7]
What Should You Do If You Are Insulin Resistant?
If you believe you are insulin resistant, you should consult your doctor to confirm and test for diabetes (HbA1c test will likely be performed). Your doctor may suggest you limit your carbohydrate intake. Research suggests the ketogenic diet can not only reduce blood glucose levels but improve insulin resistance/increase insulin sensitivity. ( [8] [9] [10] [11]
Has the Ketogenic Diet Helped You?
Have you or are you currently using the ketogenic diet for insulin resistance/type 2 diabetes? Comment and tell us your story!
References
El Sayed SA, Mukherjee S. Physiology, Pancreas. [Updated 2019 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-.
Vargas E, Carrillo Sepulveda MA. Biochemistry, Insulin Metabolic Effects. [Updated 2019 Apr 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-.
Holmes R. (1971). Carbohydrate digestion and absorption. Journal of Clinical Pathology. Supplement (Royal College of Pathologists)., 5, 10–13.
Lin CW, Yan F, Shimamura S, Barg S, Shyng SL. Membrane phosphoinositides control insulin secretion through their effects on ATP-sensitive K+ channel activity. Diabetes. 2005;54(10):2852–2858. doi:10.2337/diabetes.54.10.2852
Navale, A. M., & Paranjape, A. N. (2016). Glucose transporters: physiological and pathological roles. Biophysical reviews, 8(1), 5–9.
Wilcox G. (2005). Insulin and insulin resistance. The Clinical biochemist. Reviews, 26(2), 19–39.
InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Type 2 diabetes: Overview. 2008 Aug 27 [Updated 2018 Jan 11].
Gershuni, V. M., Yan, S. L., & Medici, V. (2018). Nutritional Ketosis for Weight Management and Reversal of Metabolic Syndrome.Current nutrition reports, 7(3), 97–106.
Westman EC, Tondt J, Maguire E, Yancy WS Jr. Implementing a low-carbohydrate, ketogenic diet to manage type 2 diabetes mellitus.Expert Rev Endocrinol Metab. 2018;13(5):263–272.
Paoli A. (2014). Ketogenic diet for obesity: friend or foe?. International journal of environmental research and public health, 11(2), 2092–2107.
Bolla, A. M., Caretto, A., Laurenzi, A., Scavini, M., & Piemonti, L. (2019). Low-Carb and Ketogenic Diets in Type 1 and Type 2 Diabetes. Nutrients, 11(5), 962.